Prevalence of Hypertension and Behavioral Risk Factors among Adults in a Rural Community of Oyo State, Southwest Nigeria
Main Article Content
Abstract
Background: Globally, there has been substantial rise in the burden of non-communicable diseases (NCDs) in the recent past and hypertension is reported as one of the most prevalent of these NCDs. Data on true prevalence of hypertension and associated factors in rural Nigerian communities are limited, hence the need for this study.
Objectives: This study assessed the prevalence and behavioral risk factors of hypertension among adults in Oko, Oyo state.
Methods: A descriptive cross-sectional study was carried out among 266 adults selected using a multistage sampling technique. Data was collected using semi-structured, interviewer-administered questionnaire. Blood pressure and anthropometric measurements were done using standard protocols. Chi-Squared test and binary logistic regression model were used for inferential statistics at p < 0.05.
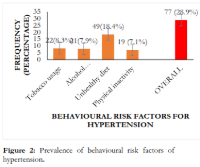
Results: The prevalence of hypertension in this study was 76 (28.6%) and 77 (28.9%) of the respondents had at least one of the behavioral risk factors of hypertension. Hypertension occurrence was significantly associated with ‘respondents’ age (AOR = 3.42; 95% CI= 1.667 – 7.009); Overweight (AOR = 3.05, 95% CI = 1.514-6.160); obese (AOR = 2.47, 95% CI = 1.057-5.793) and alcohol consumption (AOR = 0.21, 95% CI = 0.076-0.562).
Conclusion: This study found prevalence of hypertension and behavioral risk factors to be present in about a quarter of the participants. Public health professionals should implement cost-effective interventions to address hypertension and mitigate its risk factors in rural Nigerian communities.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
1. Piovani D, Nikolopoulos GK, Bonovas S. Non-Communicable Diseases: The Invisible Epidemic. J Clin Med. 2022;11(19):11–2.
2. Wang Y, Wang J. Modelling and prediction of global non-communicable diseases. BMC Public Health. 2020;20:1–13.
3. World Health Organization. World health statistics 2023: monitoring health for the SDGs, Sustainable Development Goals [Internet]. 2023. 1–119 p. Available from: [https://www.who.int/publications/book-orders](https://www.who.int/publications/book-orders).
4. Mancia G, Kreutz R, Brunström M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension the Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association. J Hypertens. 2023;41(12):1874–2071.
5. Van Oort S, Beulens JWJ, Van Ballegooijen AJ, Grobbee DE, Larsson SC. Association of Cardiovascular Risk Factors and Lifestyle Behaviors with Hypertension: A Mendelian Randomization Study. Hypertension. 2020;76(6):1971–9.
6. Kario K, Okura A, Hoshide S, Mogi M. The WHO Global report 2023 on hypertension warning the emerging hypertension burden in globe and its treatment strategy. Hypertens Res. 2024;47(5):1099–102.
7. Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in Low- and Middle-Income Countries. Circ Res. 2021;128(7):808–26.
8. Ojo OS, Malomo SO, Sogunle PT, Ige AM. An appraisal of blood pressure control and its determinants among patients with primary hypertension seen in a primary care setting in Western Nigeria. South African Fam Pract [Internet]. 2016;1(1):1–10. Available from: [http://dx.doi.org/10.1080/20786190.2016.1186367](http://dx.doi.org/10.1080/20786190.2016.1186367)
9. World Health Organization. Hypertension [Internet]. 2023 [cited 2024 Nov 14]. Available from: [https://www.who.int/news-room/fact-sheets/detail/hypertension](https://www.who.int/news-room/fact-sheets/detail/hypertension)
10. Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol [Internet]. 2021;18(November):785–802. Available from: [http://dx.doi.org/10.1038/s41569-021-00559-8](http://dx.doi.org/10.1038/s41569-021-00559-8)
11. World Health Organization. Global report on hypertension: The race against a silent killer. 2023.
12. Ranzani OT, Kalra A, Di Girolamo C, Curto A, Valerio F, Halonen JI, et al. Urban-rural differences in hypertension prevalence in low-income and middle-income countries, 1990-2020: A systematic review and meta-analysis. PLoS Med. 2022;19(8):1–19.
13. Sani RN, Connelly PJ, Toft M, Rowa-Dewar N, Delles C, Gasevic D, et al. Rural-urban difference in the prevalence of hypertension in West Africa: a systematic review and meta-analysis. J Hum Hypertens. 2024;38(4):352–64.
14. National Bureau of Statistics. Demographic Statistics Bulletin 2022. 2023.
15. Akinlua JT, Meakin R, Umar AM, Freemantle N. Current prevalence pattern of hypertension in Nigeria: A systematic review. PLoS One. 2015;10(10):1–18.
16. Adeloye D, Owolabi EO, Ojji DB, Auta A, Dewan MT, Olanrewaju TO, et al. Prevalence, awareness, treatment, and control of hypertension in Nigeria in 1995 and 2020: A systematic analysis of current evidence. J Clin Hypertens. 2021;23:963–77.
17. Oguanobi NI. Management of hypertension in Nigeria: The barriers and challenges. J Cardiol Cardiovasc Med. 2021;6:023–5.
18. Ukegbu PO, Ortutu BF, Diara S, Precious UC, Ugwunna UA. Hypertension and Associated Factors Among Community-Dwelling Rural Adults in Abia State, Nigeria. Niger J Nutr Sci. 2022;43(2):110–21.
19. Ofili MI, Ncama BP, Sartorius B. Hypertension in rural communities in Delta State, Nigeria: Prevalence, risk factors and barriers to health care. African J Prim Heal Care Fam Med. 2015;7(1):1–7.
20. Egbi OG, Ahmed SD, Madubuko R. Prevalence and biosocial determinants of hypertension in a rural population in Edo State, Southern Nigeria. African J Prim Heal Care Fam Med. 2021;13(1):1–7.
21. World Health Organization. The WHO STEPwise approach to noncommunicable disease risk factor surveillance [Internet]. 2017. Available from: [http://dx.doi.org/10.1016/j](http://dx.doi.org/10.1016/j).
22. Cesare MD, Bixby H, Gaziano T, Hadeed L, Kabudula CV, McGhie DV, et al. World Heart Report 2023: Confronting the World’s Number One Killer [Internet]. World Heart Federation. 2023. Available from: [https://world-heart-federation.org/wp-content/uploads/World-Heart-Report-2023.pdf](https://world-heart-federation.org/wp-content/uploads/World-Heart-Report-2023.pdf)
23. Govender D, Naidoo S, Taylor M. Knowledge, attitudes and peer influences related to pregnancy, sexual and reproductive health among adolescents using maternal health services in Ugu, KwaZulu-Natal, South Africa. BMC Public Health. 2019;19(928):1–16.
24. Asekun-Olarinmoye EO, Akinwusi P, Adebimpe W, Isawumi M, Hassan M, Olowe OA, et al. Prevalence of hypertension in the rural adult population of Osun State, southwestern Nigeria. Int J Gen Med. 2013;6:317–22.
25. Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: A systematic review and meta-analysis. J Hypertens. 2015;33(2):230–42.
26. Norton KI. Standards for Anthropometry Assessment. Kinanthropometry and Exercise Physiology. 2019. 68–137 p.
27. Smith CE, Metz M, Pierre JL, Rouzier V, Yan LD, Sufra R, et al. Comparison of community and clinic-based blood pressure measurements: A cross-sectional study from Haiti. PLOS Glob Public Heal [Internet]. 2022;2(9):1–14. Available from: [http://dx.doi.org/10.1371/journal.pgph.0001064](http://dx.doi.org/10.1371/journal.pgph.0001064)
28. World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013 - 2020. 2013.
29. Manley AF. Physical Activity and Health. Centers for Disease Control and Prevention. 2023.
30. Egbi OG, Ogoina D, Oyeyemi A. Prevalence of hypertension and associated factors in a rural community in Bayelsa State. Int J Res Med Sci. 2018;6(4):1106–13.
31. Okeke C, Uzochukwu B, Nawfal E, Abada E, Uzochukwu B. Prevalence Of Hypertension And Awareness Of The Causes And Effects Of Hypertension In Rural And Urban Communities Of Enugu State Nigeria. Int J Sci Technol Res [Internet]. 2017;6(12):26–32. Available from: [www.ijstr.org](http://www.ijstr.org)
32. Odili AN, Chori BS, Danladi B, Nwakile PC, Okoye IC, Abdullahi U, et al. Prevalence, awareness, treatment and control of hypertension in Nigeria: Data from a nationwide survey 2017. Glob Heart. 2020;15(1):1–13.
33. Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Prasad R. Urban rural differences in diet, physical activity and obesity in India: Are we witnessing the great Indian equalisation? Results from a cross-sectional STEPS survey. BMC Public Health [Internet]. 2016;16:1–10. Available from: [http://dx.doi.org/10.1186/s12889-016-3489-8](http://dx.doi.org/10.1186/s12889-016-3489-8)
34. Opreh OP, Olajubu TO, Akarakiri KJ, Ligenza V, Amos JT, Adeyeye AV, et al. Prevalence and factors associated with hypertension among rural community dwellers in a local government area, South West Nigeria. Afr Health Sci. 2021;21(1):75–81.
35. Ajayi IO, Sowemimo IO, Akpa OM, Ossai NE. Prevalence of hypertension and associated factors among residents of Ibadan-North Local Government Area of Nigeria. Niger J Cardiol. 2016;13(1):67–75.
36. Fuchs FD, Fuchs SC. The Effect of Alcohol on Blood Pressure and Hypertension. Curr Hypertens Rep [Internet]. 2021 Oct 1 [cited 2025 May 24];23(10):1–6. Available from: [https://link.springer.com/article/10.1007/s11906-021-01160-7](https://link.springer.com/article/10.1007/s11906-021-01160-7)
37. Aladin A, Chevli P, Ahmad MI, Rasool S, Herrington D. Alcohol Consumption and Risk of Hypertension. J Am Coll Cardiol [Internet]. 2019;73(9):12. Available from: [http://dx.doi.org/10.1016/S0735-1097(19)33774-X](http://dx.doi.org/10.1016/S0735-1097%2819%2933774-X)
38. Cecchini M, Filippini T, Whelton PK, Iamandii I, Di Federico S, Boriani G, et al. Alcohol Intake and Risk of Hypertension: A Systematic Review and Dose-Response Meta-Analysis of Nonexperimental Cohort Studies. Hypertension. 2024;81(8):1701–15.