Barriers to the Use of Antiretroviral Therapy Among HIV-Positive Pregnant Women in Awka, South-East Nigeria.
Main Article Content
Abstract
Background: Despite significant scale-up of Prevention of Mother-to-Child Transmission (PMTCT) programmes in Nigeria, adherence to antiretroviral therapy (ART) among HIV-positive pregnant women remains suboptimal, sustaining the risk of vertical HIV transmission.
Objective: This study explored the socio-cultural, health system, stigma-related, and economic factors influencing ART uptake and adherence among HIV-positive pregnant women in Awka, South-East Nigeria.
Methodology: A cross-sectional descriptive survey was conducted involving 200 HIV-positive pregnant women accessing PMTCT services in selected health facilities. Data were collected using structured interviewer-administered questionnaires and analysed with descriptive statistics including frequencies and percentages.
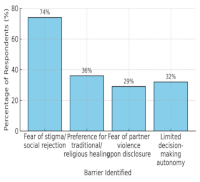
Results: Key socio-cultural barriers included fear of stigma and social rejection (74%), preference for traditional or religious healing (36%), fear of partner violence following disclosure (29%), and limited autonomy in health decisions (32%). Health system challenges identified were long clinic waiting times (61%), inadequate counselling services (48%), frequent drug stock-outs (43%), and poor integration of PMTCT with antenatal care (37%). Stigma-related and familial constraints involved limited male partner involvement (69%), pervasive community stigma (63%), and fear of losing family support (42%). Economic impediments encompassed high transportation costs (56%), inability to afford adequate nutrition (52%), opportunity costs (46%), and long distances to health facilities (39%).
Conclusion: ART adherence among HIV-positive pregnant women in Awka is impeded by intersecting socio-cultural, systemic, and economic factors. Comprehensive, multi-sectoral strategies targeting stigma reduction, male partner engagement, service integration, and economic support are critical to improving adherence and advancing elimination of mother-to-child HIV transmission.
Downloads
Article Details
Section

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.
How to Cite
References
1.Anosike V, Ogbonnaya LU, Okorie PC. Barriers to prevention of mother to child transmission of HIV services among pregnant women in South East Nigeria. Afr J Reprod Health. 2020;24(2):60-71. doi:10.29063/ajrh2020/v24i2.7
2.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. doi:10.1191/1478088706qp063oa
3.Charan J, Biswas T. How to calculate sample size for different study designs in medical research. Indian J Psychol Med. 2013;35(2):121-6. doi:10.4103/0253-7176.116232
4.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 3rd ed. Thousand Oaks (CA): Sage Publications; 2018.
5.Egwuaba EU. Utilisation of mother to child transmission of HIV services in Lokoja Metropolis, Nigeria. Sokoto J Soc Sci. 2019;9(1):135-52.
6.Egwuaba EU, Obianuo JC. Social behavioural strategies for addressing rural urban disparities in maternal health care and women’s health seeking behaviour in Asaba, Nigeria. GVU J Sci Health Technol. 2025;10(1):147-56. doi:10.5281/zenodo.15777345
7.Egwuaba EU, Offordum EK, Sunday BA. A sociocultural analysis of youth sexual behaviour and HIV/AIDS trends in Anambra State, Nigeria. Int J Sub Saharan Afr Res. 2025;3(2):131-49. doi:10.5281/zenodo.15778330
8.Egwuaba EU, Sunday BA. Challenges in health care delivery, health seeking behaviour and implementing social behavioural strategies in Awka, Nigeria. GVU J Coll Manag Soc Sci. 2025;10(1):218-35. doi:10.5281/zenodo.15863416
9.Eshun-Wilson I, Rohwer A, Hendricks L, Oliver S, Garner P. Being HIV positive and staying on antiretroviral therapy in Africa: a qualitative systematic review and theoretical model. PLoS One. 2019;14(1): e0210408. doi: 10.1371/journal.pone.0210408
10.Federal Ministry of Health Nigeria. National guidelines for HIV prevention, treatment and care, 2020. Abuja (Nigeria): Federal Ministry of Health; 2020.
11.Glanz K, Rimer BK, Viswanath K, editors. Health behavior: theory, research, and practice. 5th ed. San Francisco (CA): Jossey-Bass; 2015.
12.Gourlay A, Birdthistle I, Mburu G, Iorpenda K, Wringe A. Barriers and facilitating factors to the uptake of antiretroviral drugs for prevention of mother to child transmission of HIV in sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16(1):18588. doi:10.7448/IAS.16.1.18588
13.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59-82. doi:10.1177/1525822X05279903
14.Hampanda K. Intimate partner violence and HIV positive women’s non-adherence to antiretroviral medication for the purpose of prevention of mother to child transmission in Lusaka, Zambia. Soc Sci Med. 2016; 153:123-30.
15.Hosmer DW, Lemeshow S. Applied logistic regression. 3rd ed. Hoboken (NJ): Wiley; 2013.
16.Iwelunmor J, Airhihenbuwa CO, Okoror TA, Brown DC, BeLue R. Family systems and HIV/AIDS in South Africa. Int Q Community Health Educ. 2015;36(1):5-19. doi:10.1177/0272684X15575961
17.Kim MH, Ahmed S, Buck WC, et al. The Tingathe programme: a pilot intervention using community health workers to create a continuum of care in the prevention of mother to child transmission of HIV (PMTCT) cascade of services in Malawi. J Int AIDS Soc. 2016;19(1):20679.
18.Lincoln YS, Guba EG. Naturalistic inquiry. Newbury Park (CA): Sage Publications; 1985.
19.Nachega JB, Uthman OA, Anderson J, Peltzer K, Wampold S, Cotton MF, et al. Adherence to antiretroviral therapy during and after pregnancy in low income, middle income, and high-income countries: a systematic review and meta-analysis. AIDS. 2016;26(16):2039-52. doi:10.1097/QAD.0b013e328359590f
20.Okonji EF, Mukumbang FC, Orth Z, Vickerman Delport SA, Van Wyk B. Barriers and facilitators to HIV treatment adherence among adolescents in sub-Saharan Africa: a systematic review. AIDS Behav. 2021;25(3):745-59. doi:10.1007/s10461-020-03015-5
21.Onoka CA, Onwujekwe OE, Hanson K, Uzochukwu BS. Examining catastrophic health expenditures at variable thresholds using household consumption expenditure diaries. Trop Med Int Health. 2012;16(10):1334-41. doi:10.1111/j.1365-3156.2011. 02836.x
22.Owoyemi JO, Fatimehin OO, Egwuaba EU, Obaka P. Access and utilisation of family planning services among married couples in Kogi State, Nigeria. Cent Afr J Public Health. 2020;6(3):110-21. doi: 10.11648/j.cajph.20200603.12
23.Peltzer K, Friend du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2010; 10:111. doi:10.1186/1471-2458-10-111
24.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2(4):328-35. doi:10.1177/109019817400200403
25.UNAIDS. Global AIDS update 2021: confronting inequalities lessons for pandemic responses from 40 years of AIDS. Geneva: UNAIDS; 2021.
26.UNAIDS. Global HIV & AIDS statistics fact sheet. Geneva: UNAIDS; 2021 [cited 2025 Jul 28]. Available from: https://www.unaids.org/en/resources/fact-sheet
27.World Health Organization. Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach. Geneva: WHO; 2010 [cited 2025 Jul 28]. Available from: https://apps.who.int/iris/handle/10665/44379
28.World Health Organization. Preventing mother to child transmission (PMTCT) of HIV. Geneva: WHO; 2022.
29.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-4.