Care-Recipient Perspectives on the Responsiveness of Orthopaedic Surgical Services in a Tertiary Center in Nigeria
Keywords:
Nigeria, UPTH, University of Port Harcourt Teaching Hospital, choice of providers, autonomy, confidentiality, dignity, orthopaedic services, ResponsivenessAbstract
Background: Responsiveness optimises the system-based approach to meeting legitimate demands by healthcare recipients. This study assessed the responsiveness of orthopaedic services at the University of Port Harcourt Teaching Hospital (UPTH) from the perspectives of the care recipients.
Methods: Descriptive cross-sectional study among 442 consecutively recruited recipients of orthopaedic services at UPTH from March to June 2020. Close-ended questionnaire with responsiveness conceptualised by five constructs: dignity, autonomy, confidentiality, quality of basic amenities and choice of care provider, each measured along 4-point response scale. The internal consistency reliability of the responsiveness scale was determined by the Cronbach’s alpha coefficient. Descriptive (frequency, percentages, bar charts) and inferential (ordinal logistic regression) statistics were conducted and p-values ≤ 0.05 were considered statistically significant.
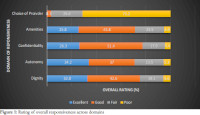
Results: Response rate was 97.3% and the Cronbach’s alpha coefficient for the responsiveness scale was 0.83. Participants’ mean age was 38.5±14.8years with more being males (55.8%), privately employed (34.9%) and completed secondary education (82.5%). Proportion of respondents who gave excellent ratings across responsiveness domains were dignity (32.8%), autonomy (34.2%), confidentiality (26.3%), amenities (25.8%) and no excellent rating for choice of provider. Marital, employment and visit status were the most consistent factors associated with feedback on autonomy, choice of providers, confidentiality domains.
Conclusion: More orthopaedic patients were pleased with the level of autonomy and dignity than choice of providers and quality of basic amenities. There is the need for enhanced responsiveness of orthopedic services to meeting the unique needs of patients and achieving improved quality of care and patient outcomes.
References
World Health Report: Health systems improving performance. 2000, Geneva, Switzerland: World Health Organization
Mirzoev T, Kane S. What is health systems responsiveness? Review of existing knowledge and proposed conceptual framework. BMJ global health. 2017 Oct 1;2(4):e000486.
Valentine NB, de Silva A, Kawabata K, Darby C, Murray CJL, Evans DB, Murray C, Evans D: Health systems performance assessment: debates, methods and empiricism Geneva. Health System Responsiveness: concepts, domains and operationalization. 2003, Geneva, Switzerland: World Health Organization, 573-595.
Ogaji DS, Egu CB, Nwakor-osaji M, Smart AC, Anyiam EF, Diorgu FC. Responsiveness of primary health care services in Nigeria: The
patients’ perspective. Patient Experience Journal. 2020;7(3):146-54.
Gani A, Bhat S, Gupta A. Pattern & Prevalence of Orthopaedic Outdoor patients at a tertiary level care Hospital in Jammu, India. JK Science. 2016 Jul 1;18(3):155-158
Murray CJL, Frenk J: Ranking 37th — Measuring the Performance of the U.S. Health Care System. N Engl J Med. 2010, 362 (2): 98-99.
Doi:10.1056/NEJMp0910064.
Figueras J, Saltman RB, Busse R, Dubois HFW: Patterns and performance in social health insurance systems. Social health insurance systems in Western Europe. Edited by: Saltman RB, Busse R, Figueras J. 2004, Berkshire, New York: Open University Press, 81.
Onuminya JE. The role of traditional bone setters in primary fracture care in Nigeria. S Afr Med J 2004; 94(8): 652 – 658.
Oyebola DD. Yoruba traditional bonesetters: the practice of orthopaedics in a primitive setting in Nigeria. J Trauma 1980; 20: 312 – 322.
Ekere AU. A review on the challenge of traditional bone setting to orthodox ortho/trauma practice in the developing world. Niger Health J 2004; 4: 219 – 223
Udosen AM, Otei OO, Onuba O. Role of traditional bone setters in Africa: experience in Calabar, Nigeria. Ann Afr Med 2006; 5(4): 170 – 173.
Nunes B, Esteves MJ. Therapeutic itineraries in rural and urban areas: a Portuguese study. Rural Remote Health 2006; 6(1): 394.
Alonge TO, Dongo AE, Nottidge TE, Omololu AB, Ogunlade SO. Traditional bonesetters in southwestern Nigeria – friends or foes? West Afr J Med 2004; 23(1): 81 – 84.
University of Port Harcourt Teaching Hospital, 5- year strategic plan (2021 - 2026), UPTH, Alakahia
Cochran, W. G. (1977). Sampling techniques (3rd ed.). New York: John Wiley & Sons.
Ajayi IO, Olumide EA, Oyediran O. Patient satisfaction with the services provided at a generaloutpatients’ clinic, Ibadan, Oyo State, Nigeria. Afr J Med Med Sci 2005; 34:133-40
Bramesfeld A, Wedegartner F, Elgeti H, Bisson S. How does mental healthcare perform in respect to service users’ expectations? Evaluating inpatient and outpatient care in Germany with the WHO responsiveness concept. BMC Health Serv Res 2007; 7:99
Chariatte, V., Berchtold, A., Akre, C., Michaud, P., A., & Suris, J.C. (2007). Missed appointments in an outpatient clinic for adolescents, an approach to predict the risk of missing. J Adolesc Health, 43: 38–45. 10.1016/j.jadohealth.12.017
Onyemaechi NO, Lasebikan OA, Elachi IC, Popoola SO, Oluwadiya KS. Patronage of traditional bonesetters in Makurdi, north-central
Nigeria. Patient preference and adherence. 2015 Feb 9:275-9.
Yu J, Samuel LT, Yalçin S, Sultan AA, Kamath AF. Patient-recorded physician ratings: what can we learn from 11,527 online reviews of orthopedic surgeons? The Journal of Arthroplasty. 2020 Jun 1;35(6):S364-7.
Syed, M. A., Azim, S. R., & Baig, M. (2019) Frequency of orthopedic problems among patients attending an orthopedic outpatient
department: a retrospective analysis of 23 495 cases. Ann Saudi Med, 39(3): 172-177 DOI: 10.5144/0256-4947.2019.172
Dixon, A., Robertson, R., & Bal, R., (2010). The experience of implementing choice at point of referral. A comparison of Netherlands and England. Health Econ Policy law,5: 295-317
Ranerup, A., Noren, L., & Sparud-Linden, C., (2011). Decision support systems for choosing a primary health care provider in Sweden. Patient Educ Couns, 86: 342-347.
Ogaji DS. Patient-focused quality improvement in primary health care: opportunities with the patient evaluation scale. Journal of Community Medicine and Primary Health Care. 2017 Nov 2;29(2):84-96.
Mohammed S, Bermejo JL, Souares A, Sauerborn R, Dong H. Assessing responsiveness of health care services within a health insurance scheme in Nigeria: Users’ perspectives. BMC Health Serv Res. 2013;13(1):502. https://doi.org/10.1186/1472-6963-13-502
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Journal and Publisher

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
The Journal is owned, published and copyrighted by the Nigerian Medical Association, River state Branch. The copyright of papers published are vested in the journal and the publisher. In line with our open access policy and the Creative Commons Attribution License policy authors are allowed to share their work with an acknowledgement of the work's authorship and initial publication in this journal.
This is an open access journal which means that all content is freely available without charge to the user or his/her institution. Users are allowed to read, download, copy, distribute, print, search, or link to the full texts of the articles in this journal without asking prior permission from the publisher or the author.
The use of general descriptive names, trade names, trademarks, and so forth in this publication, even if not specifically identified, does not imply that these names are not protected by the relevant laws and regulations. While the advice and information in this journal are believed to be true and accurate on the date of its going to press, neither the authors, the editors, nor the publisher can accept any legal responsibility for any errors or omissions that may be made. The publisher makes no warranty, express or implied, with respect to the material contained herein.
TNHJ also supports open access archiving of articles published in the journal after three months of publication. Authors are permitted and encouraged to post their work online (e.g, in institutional repositories or on their website) within the stated period, as it can lead to productive exchanges, as well as earlier and greater citation of published work (See The Effect of Open Access). All requests for permission for open access archiving outside this period should be sent to the editor via email to editor@tnhjph.com.